When bacteria evolve mechanisms against more than one antibiotic, they are referred to as “multidrug-resistant bacteria.” These type of bacteria present two challenges: they are difficult to treat and they can help other bacteria develop multidrug resistance, enabling them to spread further. Newer strains present greater danger.
Over 2.8 million people get infections caused by antibiotic-resistant bacteria each year.
35,000 people die from these evolved strains in the U.S. alone.
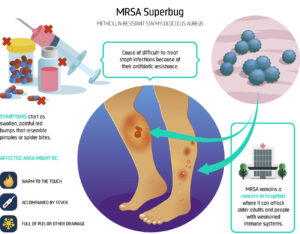
Methicillin-Resistant Staphylococcus aureus (MRSA) is a type of staph bacteria that has become resistant to many of the antibiotics used to treat ordinary staph infections. Most MRSA infections occur in pathogen-rich environments such as hospitals or other healthcare settings, including nursing homes and dialysis centers.
Healthcare-Associated MRSA (HA-MRSA) infections are commonly associated with invasive procedures or devices, such as surgeries, intravenous tubing, or artificial joints.
Community-Associated MRSA (CA-MRSA) infections are painful skin infection and can spread via contact with a contaminated wounds or by sharing personal items, such as towels or razors, that have touched infected skin.
Livestock-Associated MRSA (LA-MRSA) is an emerging problem in many parts of the world. Prolonged, repeated contact with affected livestock causes at a higher risk of becoming colonized with LA-MRSA.
Approximately 86% of all invasive MRSA infections are healthcare-associated. From 2008-2012, approximately 9% of patients with a clinical MRSA infection died and 25% of patients with a MRSA bloodstream infection died 30 days after the date of positive culture (Canada PHA).
1% of the global population, are colonized with MRSA. That means that bacteria is present but not currently causing an infection. Close contact with MRSA-infected people or animals increases the risk of infection.